Stages of Chronic Kidney Disease
chronic Kidney Disease is classified into five stages, based on the level of kidney function and the presence of kidney damage:
Stage 1
- GFR (Glomerular Filtration Rate): 90 mL/min or higher.
- Kidney Damage: Presence of kidney damage (e.g., proteinuria or hematuria) with a normal or increased GFR.
- Symptoms: Generally asymptomatic; kidney function is normal or near normal.
Stage 2
- GFR: 60-89 mL/min.
- Kidney Damage: Evidence of kidney damage with a mild decrease in GFR.
- Symptoms: Mild symptoms may start to appear; risk of progression to more advanced stages increases.
Stage 3
- GFR: 30-59 mL/min.
- Kidney Damage: Moderate decrease in kidney function.
- Symptoms: May include fatigue, swelling, and changes in urine output. Some complications, such as anemia or bone disease, may begin.
Stage 4
- GFR: 15-29 mL/min.
- Kidney Damage: Severe decrease in kidney function.
- Symptoms: More pronounced symptoms, including significant fluid retention, electrolyte imbalances, and worsening of anemia. Preparation for dialysis or kidney transplant may be needed.
Stage 5
Primary Causes of Chronic Kidney Disease
Chronic Kidney Disease (CKD) is closely linked to diabetes, which is one of its major causes. Diabetes affects the kidneys by causing high blood sugar levels to damage the tiny blood vessels in the kidneys, especially in the glomeruli, which are the filtering units. This damage impairs the kidneys’ ability to filter waste from the blood effectively.
Over time, as diabetes continues to damage these blood vessels, the kidneys lose their ability to function properly. This condition, known as diabetic nephropathy, often develops gradually. In the early stages, it might not show any obvious symptoms, but as it progresses, symptoms like excess protein in the urine, high blood pressure, and swelling can appear.
High blood pressure, which is common in people with diabetes, can further worsen kidney damage. This creates a cycle where high blood sugar and high blood pressure continually damage the kidneys, leading to a faster decline in kidney function.
Managing diabetes effectively is crucial to slowing down the progression of CKD. Good control of blood sugar levels, along with medication, diet, and lifestyle changes, can help protect the kidneys. Without proper management, diabetes can lead to more severe kidney problems.
Globally, diabetes is a major health issue, with around 537 million adults affected as of recent estimates. In the United States, about one-third of people with diabetes also have CKD, highlighting how common this complication is among diabetics. This underscores the importance of managing diabetes to prevent or slow the onset of kidney disease.
Hypertension and Its Impact on the Kidneys
Hypertension, or high blood pressure, has a significant impact on kidney health. When blood pressure is consistently elevated, it puts extra strain on the blood vessels throughout the body, including those in the kidneys. Over time, this can damage the delicate blood vessels in the glomeruli, the filtering units of the kidneys.
This damage impairs the kidneys’ ability to effectively filter waste and excess fluids from the blood. As a result, high blood pressure can lead to the development or worsening of chronic kidney disease (CKD).
Managing blood pressure is crucial in preventing CKD. Effective management typically involves lifestyle changes such as adopting a heart-healthy diet, increasing physical activity, reducing sodium intake, and avoiding excessive alcohol consumption.
Glomerulonephritis
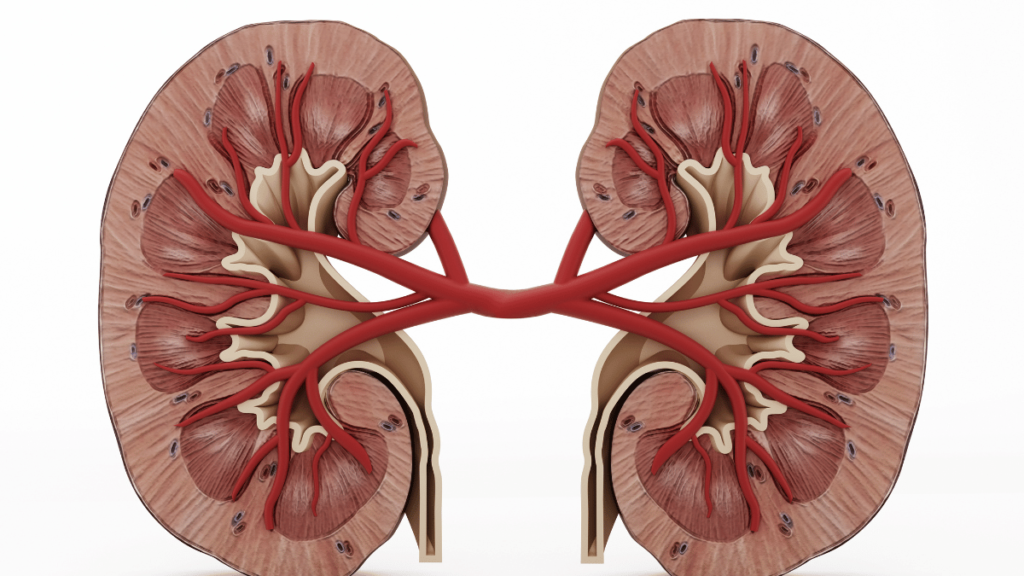
Glomerulonephritis refers to a group of kidney conditions characterized by inflammation of the glomeruli. There are several types of glomerulonephritis, each with different causes and effects. Some common types include:
- Acute Glomerulonephritis: Often develops suddenly, potentially following an infection such as strep throat. It can lead to symptoms like blood in the urine, swelling, and high blood pressure.
- Chronic Glomerulonephritis: Develops gradually over years and can lead to long-term kidney damage. It may be associated with conditions like autoimmune disorders.
- IgA Nephropathy (Berger’s Disease): Caused by the buildup of IgA antibodies in the kidneys, leading to inflammation and damage.
Symptoms of glomerulonephritis can vary but often include blood or protein in the urine, swelling in the legs and ankles, high blood pressure, and reduced urine output. Diagnosis typically involves urine tests, blood tests, and sometimes a kidney biopsy to assess the extent of kidney damage.
Polycystic Kidney Disease (PKD)
Polycystic Kidney Disease (PKD) is a genetic disorder characterized by the growth of numerous cysts in the kidneys. These cysts can vary in size and may eventually lead to kidney damage and kidney failure.
PKD is inherited, usually in an autosomal dominant pattern, meaning that an individual only needs one copy of the mutated gene from a parent to develop the disease. There are two main types of PKD:
- Autosomal Dominant PKD (ADPKD): The most common form, usually developing in adulthood. Symptoms often include high blood pressure, back pain, and kidney stones.
- Autosomal Recessive PKD (ARPKD): A rarer form, often diagnosed in infancy or early childhood. It typically causes more severe kidney damage and can lead to complications early in life.
Treatment for PKD focuses on managing symptoms and slowing disease progression. This can include blood pressure management, pain relief, and in severe cases, dialysis or kidney transplantation.
Risk Factors Contributing to CKD
Several risk factors contribute to the development and progression of chronic kidney disease. Family history and genetics play a significant role, as having a family member with CKD increases one’s risk of developing the condition. Age is another factor, with older adults being more susceptible to CKD. Gender also plays a role, as CKD is slightly more common in women than in men.
Lifestyle factors such as diet, smoking, and physical activity have a considerable impact on kidney health. A diet high in sodium and processed foods, smoking, and lack of exercise can all contribute to kidney damage. Managing these lifestyle factors is crucial for preventing CKD.
Other medical conditions, such as heart disease and autoimmune disorders, can also contribute to the development of CKD. Conditions like diabetes and hypertension often coexist with heart disease, compounding the risk of kidney damage.
Secondary Causes and Contributing Conditions

Secondary causes of CKD include urinary tract obstruction, which can occur due to kidney stones or tumors blocking the urinary tract. This obstruction causes pressure buildup in the kidneys, leading to damage and impaired function.
The prolonged use of certain medications can also impact kidney function. Nonsteroidal anti-inflammatory drugs (NSAIDs) and some antibiotics, when used long-term or in high doses, can be harmful to the kidneys.
Infections and inflammatory diseases can contribute to CKD as well. Chronic kidney infections, such as pyelonephritis, can lead to kidney damage over time if not properly treated.
Prevention and Management of Chronic Kidney Disease
Early detection and screening are essential for preventing and managing chronic kidney disease. Regular check-ups with a healthcare provider can help identify kidney issues before they become severe.
Lifestyle modifications are a critical component of CKD prevention and management. These include adopting a balanced diet low in sodium and high in fruits and vegetables, engaging in regular physical activity, quitting smoking, and managing weight.
Medical treatments and therapies aim to manage underlying conditions such as diabetes and hypertension, which are critical in slowing the progression of CKD. Medications to control blood pressure, manage blood sugar levels, and reduce proteinuria can be part of a comprehensive treatment plan. For advanced CKD, treatments such as dialysis or kidney transplantation may be necessary.
Overall, proactive management and lifestyle adjustments play a crucial role in preventing the onset and progression of chronic kidney disease.
Conclusion
Chronic Kidney Disease (CKD) is a serious and progressive condition that can arise from various causes, with diabetes and hypertension being among the most significant contributors. Diabetes damages the kidneys through high blood sugar levels that harm the delicate filtering units, while high blood pressure exacerbates this damage by stressing the kidney’s blood vessels. Both conditions create a cycle of worsening kidney function if not properly managed.
Other key factors influencing CKD include glomerulonephritis, a group of diseases causing inflammation in the kidneys’ filtering units, and Polycystic Kidney Disease (PKD), a genetic disorder leading to cyst formation and kidney damage. The risk of CKD is also heightened by factors such as family history, age, gender, lifestyle choices (like diet and smoking), and other medical conditions such as heart disease and autoimmune disorders.
Secondary causes of CKD, such as urinary tract obstruction, prolonged medication use, and chronic infections, further complicate kidney health. Early detection through regular screening, along with proactive management of underlying conditions, is crucial for slowing the progression of CKD.
FAQ
What causes chronic kidney disease?
Chronic kidney disease can be caused by diabetes, high blood pressure, glomerulonephritis, and polycystic kidney disease. Other factors include urinary tract obstructions, prolonged medication use, and chronic infections.
How does diabetes lead to chronic kidney disease?
Diabetes damages the blood vessels in the kidneys, impairing their ability to filter waste due to prolonged high blood sugar levels, which leads to diabetic nephropathy.
What role does high blood pressure play in CKD?
High blood pressure damages kidney blood vessels, making it difficult for the kidneys to filter waste and worsening existing kidney damage.
What is glomerulonephritis, and how does it affect the kidneys?
Glomerulonephritis is inflammation of the kidney’s filtering units, which impairs kidney function and can cause symptoms like blood in the urine and high blood pressure.
What is Polycystic Kidney Disease (PKD)?
PKD is a genetic disorder where multiple cysts form in the kidneys, leading to kidney damage over time. There are two main types: Autosomal Dominant and Autosomal Recessive PKD.